Thoracic osteochondrosis is rare in clinical practice. It used to be mainly diagnosed in the elderly, but today it is commonly found in those under the age of 35. The pathology develops more often in women than in men. This degenerative-dystrophic disease is difficult to diagnose because severe symptoms do not appear until later stages.
Furthermore, the symptoms of this disorder can easily be mistaken for signs of impaired lung and heart function. This disease cannot go without treatment, as it can cause curvature of the spine, the development of persistent pain syndrome, and other complications that can negatively affect the quality of life of the person.
What is thoracic osteochondrosis?

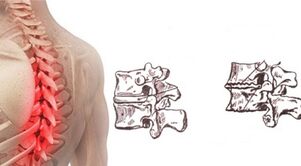
In the international classification of diseases, this pathological condition has an ICD-10 code - M42. Thoracic osteochondrosis is much less common than cervical or sacral. It's not a coincidence. Because of the presence of a rigid rib cage in this part of the body, this part of the spine is physiologically less mobile.
The thoracic region contains more vertebrae than the cervical and lumbar spine, but in this part of the spine the intervertebral discs are thinner. These anatomical features help reduce the mobility of this part of the spine, making it less prone to injury.
However, if you are exposed to a number of adverse factors, osteochondrosis can develop. At first there are signs of damage to a disc, but in the future, other elements may be involved in the pathological process. As the disease progresses, bone elements and the ligaments and muscles that support the spine become damaged.
Degenerative-dystrophic processes in the chest area grow more slowly. It often takes years for the fiber rings of damaged intervertebral discs to be so badly damaged that protrusions and hernias appear.
Severe clinical manifestations occur after a critical decrease in disc height and root entrapment. This can lead not only to dorsago, that is, short-term pain attacks in the chest area, but also to a violation of the innervation of internal organs. It is much more difficult to treat pinched nerve roots that extend in this area.
Reasons for development
In most cases, spinal problems don't appear suddenly. A disease like osteochondrosis is no exception in this regard. This pathology, affecting the intervertebral discs, is the result of long-term degenerative-dystrophic processes. In most cases, it is impossible to pinpoint exactly what caused the disorder to develop. Factors that can provoke the occurrence of thoracic spine osteochondrosis include:
- congenital or acquired deformities of the spine;
- overweight;
- Overloading the spine during pregnancy;
- infectious diseases;
- hypothermia;
- metabolic disorders;
- hormonal disorders;
- chronic stress;
- bad habits;
- connective tissue diseases;
- dysplastic changes;
- Postural disorders;
- unhealthy diet;
- injuries.
The withdrawal has a negative effect on the state of the spine. People who lead sedentary lifestyles are more likely to have breast osteochondrosis. In addition, age-related changes and a slowdown in metabolism seen in patients over the age of 55 contribute to the occurrence of these disorders.
Genetic predisposition can be a factor that can provoke the development of pathology. The genes that create the conditions for breast osteochondrosis to develop have not yet been identified, but it is more commonly diagnosed in people with a family history of cases of the disease.
Symptoms and Signs
The clinic for this pathological condition depends on the stage of neglect of the process, the extent to which the lesion of the intervertebral disc appeared and the age of the patient. There are no specific signs in the early stages of development, but general symptoms can appear periodically. In the initial stages of development, the disease often only manifests itself with the onset of cold weather or after physical overload. The first manifestations of the development of osteochondrosis of the chest region include:
- quick fatigue;
- pain and pressure in the back;
- muscle cramps;
- cold extremities.
As the disease progresses, the patient's condition worsens. There is painful pain in the chest. They occur particularly often against the background of prolonged stay in one position or with sudden movements. In addition, severe pain syndrome can occur when lifting weights. Turning the trunk can cause increased pain. The presence of osteochondrosis is also indicated by the appearance of dull pain in the area of the shoulder blades.
Often, osteochondrosis of the chest region is accompanied by the appearance of an abnormal curvature. In severe cases, the patient may develop a hump. In addition, this disease can cause pain on deep breaths and on exhalations.
When the nerve roots become pinched, there is often a feeling of numbness in the upper limbs and skin of the upper body. Due to the violation of innervation and blood circulation, a feeling of goose bumps appears on the skin. Feet and hands are always cold. Limb tenderness may be present. In advanced cases, this disease can lead to the appearance of symptoms of damage to other organs as a result of a violation of their innervation. In the final stages of the process, it is possible that:

- intercostal neuralgia;
- stool disorders;
- flatulence;
- heartburn and nausea;
- itching and burning in the feet;
- violations of the reproductive system;
- asthma attacks.
As the pathology progresses, a person's ability to work decreases. Physical activity is minimized. In the future, this disorder can create conditions for the development of severe complications. The risk of pathological fractures increases. The curvature of the spine leads to compression of the organs in the chest.
If the course is unfavorable, the disease progresses with an injury to the heart muscle and a decrease in lung volume. Most often, such severe complications are associated with widespread osteochondrosis, which affects several intervertebral discs at the same time.
Degree of osteochondrosis of the chest
The existing classification divides the development process of this pathological condition into 4 degrees. Each of them is characterized by the presence of a number of changes in the structure of the intervertebral discs, vertebrae and other elements that make up this part of the spine.
First degree
At the first degree of pathology there are no pronounced clinical manifestations, but specific changes in the structure of the intervertebral discs can be revealed already with a comprehensive diagnosis. The ring of fibers, receiving less moisture and nutrients, gradually loses its elasticity. Microcracks often form on the tissues into which the nucleus pulposus is forced out. Shifting the intervertebral discs into the spinal canal is possible. Projections are formed. There is no evidence of a rupture of the annulus fibrosus.
Second degree
With the transition of the disease to the second degree, the first clinical manifestations are observed. Occasionally, patients experience pain and other neurological symptoms. When carrying out specific diagnoses, signs of a decrease in the elasticity of the tissues that make up the annulus fibrosus can be detected. The cartilage becomes very thin, which increases the risk of hernia. The height of the intervertebral discs decreases, causing the structures of the spine to develop abnormal mobility.
Third degree
In the third stage, changes in the structure of the intervertebral discs become so pronounced that the first signs of the development of kyphosis or scoliosis appear. At this stage of the process, the damaged annulus fibrosus often ruptures. This phenomenon is associated with the exit of the nucleus pulposus beyond the intervertebral disc. A hernia that forms can compress the nerve roots or the spinal cord, depending on the direction of the protrusion. There is severe pain and neurological disorders. The mobility of the spine increases, which creates conditions for injuries and fractures.
Fourth degree
With the transition of the pathology to the fourth stage of development, the structure of the intervertebral discs is so severely disturbed that they no longer perform the amortization function. The annulus fibrosus and the nucleus pulposus lose their elasticity. These elements begin to ossify. Due to the violation of the amortization function of the intervertebral discs, the vertebrae suffer from excessive stress.
At the edges of the vertebrae next to the damaged intervertebral disc, osteophytes, that is, bone growth, begin to grow rapidly. The surrounding ligaments are involved in the pathological process. They lose their elasticity and no longer support the spine properly. In addition, at this stage of the development of the pathological process, the work of the muscular apparatus is disrupted.
Make a diagnosis
If signs of this disorder appear, the patient should be consulted by a neurologist and orthopedic surgeon. First of all, the doctor conducts an external examination and collects an anamnesis. Laboratory tests that are often prescribed in diagnosing this disease include blood and urine tests. To obtain information about the presence of defects in the structure of the spine, x-rays are taken. This research shows:
- Decrease the disc height;
- jagged edges of elements;
- hernia;
- change in the vertebral bodies;
- forms osteophytes and so on.
In order to clear up the errors in the structure of the disc, a discography is assigned. This study allows you to identify the uneven contours of the nucleus pulposus, assess the degree of disc destruction, and the decrease in tissue density. CT and MRI are often done for better visualization. Considering that the clinical manifestations of thoracic osteochondrosis are similar to symptoms of coronary artery disease, electrocardiography is often prescribed to distinguish these conditions.
Treatment options
This pathological condition requires complex treatment. First of all, patients are selected drugs that will help eliminate symptomatic manifestations and improve the nutrition of the intervertebral discs. Drug treatment should be supplemented with physiotherapy and exercise therapy. As a supplement, you can use some folk remedies. In addition, it is recommended to follow a certain diet.
Medicines
If the pain syndrome is severe, the patient is advised to keep to bed rest. This will reduce the intensity of the pain. To eliminate discomfort, analgesics and NSAIDs are often prescribed. If the pain syndrome manifests too much, blockages may be required. Glucocorticosteroids are often prescribed to help relieve pain from this disease.
Chondroprotectors are prescribed to improve the nutrient and water saturation of the intervertebral discs. In some cases, anticonvulsants and muscle relaxants are prescribed in short courses. These drugs help relieve muscle spasms. If necessary, diuretics are prescribed to eliminate soft tissue edema. To improve the condition of the compressed nerve endings, the patient needs B vitamins.
Physiotherapy and massage
Therapeutic exercise and massage are the most important components of osteochondrosis treatment, but can only be used after symptoms have been suppressed with medication. Properly selected exercises will help improve lung ventilation and strengthen the muscle corset that supports the spine.
First, all the necessary exercises must be learned under the supervision of a movement therapist. In the future, the patient can do exercises at home. People with this condition may be advised to take pool lessons.
Massage helps eliminate muscle hypertension and improve soft tissue nutrition. So that the procedures do not harm, they need to be carried out by a specialist. In most cases, a classic massage is performed, in which the problem area is rubbed, smoothed and pinched one by one. Acupressure and segment massage can be of great benefit. These techniques concern the impact on pain points. They improve blood circulation and lymphatic drainage. In most cases, it is enough for patients to have procedures 2-3 times a week.
Acupuncture
With this method, needles are placed on parts of the patient's body. This method allows you to quickly get rid of muscle spasms and pain. Acupuncture procedures should be performed by a professional in the matter. When a specialist does this, the procedure is almost painless. Acupuncture is contraindicated for people suffering from oncological diseases and mental disorders. It is not recommended to use this method of treating osteochondrosis in severe inflammatory processes.
Manual therapy
Manual therapy helps restore the correct anatomical position of the vertebrae. In addition, this method helps reduce the intensity of pain and muscle spasms. This effect helps to restore the ligamentous apparatus. Such procedures can slow the development of this pathological condition. The duration of the course of manual therapy is selected individually for the patient.
Post-isometric relaxation technique

Post-isometric relaxation procedures are a special technique in which all muscles surrounding the spine are tensed and then relaxed.
Such exercises should be performed under the supervision of a specialist who will be able to assess the correctness of movement and the severity of muscle tension. This method allows you to quickly get rid of pain and restore normal muscle and ligament function.
Folk Remedies
It is impossible to treat osteochondrosis with only folk remedies, since this approach can lead to a worsening of the course of the disease. It is best to use a variety of formulations based on herbs and other natural ingredients as a complement to traditional therapies. You should seek medical advice on the appropriateness of using this or that folk remedy before starting its use.
Celery root
It is believed that properly cooked celery root helps saturate the cartilage tissue with nutrients and water. To prepare this product, 1 root should be thoroughly chopped and poured 1 liter of boiling water. You must insist on the composition for at least 8 hours. After this time, you need to strain the product and take 1 tsp. 3 times a day before meals.
Sunflower root
A decoction of the sunflower root is often used to treat osteochondrosis of the cervical spine. To prepare this product you will need about 1 glass of chopped vegetable ingredient, pour 3 liters of water. The mixture must be boiled for 3-5 minutes. After that, the remedy should be cooled and taken in the form of tea for several days. To improve the taste of the drink, you can add honey. It is better to keep the rest of the drug in a thermos.
Home ointment
A simple homemade ointment can be used for rubbing with osteochondrosis. To make this product, you need to melt about 150 grams of pork fat in a water bath. After that, 2 tbsp should be entered. l. natural wax.
The composition must be boiled for at least 20 minutes. After that, 1 tbsp should be added to the heated mixture. l. Fir oil. The product must be boiled for another 20 minutes. Last but not least, 1 tbsp is added to the mixture 2-3 minutes before removing the container. l. Ammonia. The finished composition must be distributed in jars. Keep homemade ointment in the refrigerator.
Diet for breast osteochondrosis
Patients with osteochondrosis of the chest region need a balanced diet. A sufficient amount of high protein foods should be included in the diet. It is advisable to regularly consume dishes that contain a large amount of chondroitin, including aspic made from fish, jellied meat, and so on. Fermented dairy products, vegetables and fruits must necessarily be included in the diet. Dishes should be steamed or baked. Fatty and fried foods should be avoided. It is advisable to eat small portions, but take it often. This will avoid overeating.
anger: what to do?
In the acute phase of the course of the disease, it is desirable to reduce activity to a minimum. If possible, you should avoid poses that increase pain syndrome. First aid in the worsening of osteochondrosis involves the use of drugs that reduce the severity of edema, inflammation, and pain. The patient is advised to rest in bed. It is advisable to follow a frugal diet during this time. Only after the symptoms have been eliminated can you begin exercise therapy and physical therapy.
Forecast
Now this disease can only be cured in the early stages of development. If diagnosed late, therapy aims to eliminate symptoms and improve spine mobility. In some cases, surgical treatment is required. With an integrated approach to therapy, a person suffering from this pathology can lead a full-fledged lifestyle without experiencing pain and other neurological disorders.
Prevention
To prevent the development of this pathological condition, it is recommended to avoid sudden heavy lifting. You should always adapt to the weather and avoid hypothermia. Also, to prevent osteochondrosis, one should combat hypodynamics and monitor posture. As part of the prevention of this pathology, it is recommended to eat right and carefully monitor your weight.



























